First outbreak of deadly, treatment-resistant fungal infection reported in Washington State
02/29/2024 / By Olivia Cook
Four cases of Candida auris infection were reported this February in Washington State at the Kindred Hospital, a long-term acute care facility on First Hill in Seattle.
Public Health — Seattle & King County was notified of the first case on Jan. 10, after a proactive screening program called the Partners for Patient Safety Program detected the infection in a patient who was recently admitted to Kindred. Additional screening of other patients identified two new cases on Jan. 22 and a fourth case with links to Kindred Hospital on Jan. 26.
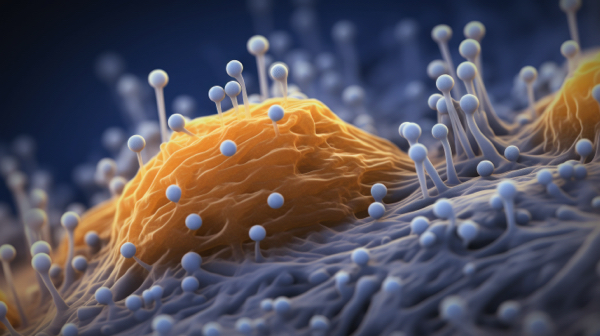
According to the Centers for Disease Control and Prevention (CDC), the fungus C. auris can easily spread from person to person in hospitals and nursing homes, causing infections in the bloodstream, ear, urinary tract and wounds. While the fungus is not a threat to healthy people, an infected individual can carry C. auris somewhere in his body without knowing it because it doesn’t make him sick. The CDC refers to this as “colonization.”
Dr. Meagan Kay, deputy chief of Public Health — Seattle & King County, said patients who have a lot of underlying conditions and/or medical devices in place are at high risk of acquiring this infection, especially in healthcare settings. “The concern when you get “colonized” is that you are at higher risk for acquiring an infection that can lead to serious outcomes and death – even at least 30 percent of the time,” explained Kay.
According to CDC data published in the Annals of Internal Medicine, the very first C. auris infection in the U.S. was reported in 2016, and the pathogen has spread rapidly since, with a total of 3,270 clinical cases (in which infection was present) and 7,413 screening cases (in which the fungus was detected but did not cause infection) reported through Dec. 31, 2021. The first case of C. auris infection in Washington State was reported in July 2023.
According to Kay, it is “nearly impossible to eliminate this organism because it persists in the environment for even weeks at a time and it’s highly transmissible.” (Related. Fungal brain infection that killed Texas woman and hospitalized four others linked to unsterilized equipment and cheap cosmetic surgeries in Mexico.)
Research on Candida auris
C. auris, a type of fungus that can cause potentially deadly bloodstream infections, can also infect the respiratory system, the central nervous system and the skin.
“Traditionally, patients who get Candida infections are patients who have received a lot of antibiotics or are immuno-suppressed for other reasons. And, they are the people that are most at risk of getting C. auris,” explained infectious disease physician and epidemiologist Dr. Anthony D. Harris of the University of Maryland School of Medicine.
The CDC said cases of C. auris are growing in the United States. The fungus is resistant to common anti-fungal drugs, can survive on clothing and hard surfaces, and often spreads in hospital settings.
Harris noted: “The healthcare worker is the ‘transient vector’ – transiently getting it on their clothing or their hands and then they move it from one room to another or through shared equipment.”
The University of Maryland is one of 11 epicenters in the U.S. currently participating in a CDC study of C. auris. The university is also gathering data to help the State Health Department determine the prevalence of Candida auris in Maryland.
Superfungus infections have risen in many parts of the U.S.
In October 2022, the World Health Organization (WHO) warned that C. auris infection has become rampant in healthcare settings in recent years, where it has killed up to a third of infected patients, becoming a “major threat” to public health.
“Emerging from the shadows of the bacterial antimicrobial resistance pandemic, fungal infections are growing and are ever more resistant to treatments, becoming a public health concern worldwide. Fears of widespread infections have been made worse because C. auris is becoming resistant to drugs, and there is currently no vaccine to prevent the infection,” said Dr. Hanan Balkhy, WHO Assistant Director-General for Antimicrobial Resistance (AMR).
“With a kill rate of 60 percent, case numbers of Candida auris infections more than tripled across America between 2020 and 2021 – from 1,310 in 2020 to 4,041 in 2021. Cases of multidrug-resistant strains also became more common,” reported the American College of Physicians (ACAP) in March 2023.
From January to December 2022, more than 2,300 clinical cases and more than 5.700 screening cases have been recorded in the U.S., with Nevada having the highest number of cases, followed by California and then Florida, according to the CDC.
Visit Outbreak.news for more stories like this.
Watch this video about Washington State hospitals taking precautions after confirming the first case of Candida auris fungal infection in a patient.
This video is from the Daily Videos channel on Brighteon.com.
More related stories:
Rare fungal infection spreads at Michigan paper mill, affecting 100 workers.
Oregon hospital reports outbreak of rare fungal superbug.
Fungal meningitis outbreak causes 7th death, CDC wants everyone to get “tested.”
Sources include:
Submit a correction >>
Tagged Under:
big government, Candida auris, CDC, chaos, colonization, Dangerous, fungal infections, health science, hospital infections, kill vectors, national security, outbreak, panic, Seattle, superbugs, Washington state
This article may contain statements that reflect the opinion of the author
RECENT NEWS & ARTICLES
COPYRIGHT © 2017 CDC NEWS